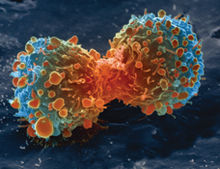
False-color scanning electron micrograph of a lung cancer cell dividing
Similar to many other cancers, lung cancer is initiated by activation of oncogenes or inactivation of tumor suppressor genes.Carcinogens cause mutations in these genes which induce the development of cancer.
Mutations in the K-ras proto-oncogene are responsible for 10–30% of lung adenocarcinomas. About 4% of non-small-cell lung carcinomas involve an EML4-ALK tyrosine kinase fusion gene.
Epigenetic changes—such as alteration of DNA methylation, histone tail modification, or microRNA regulation—may lead to inactivation of tumor suppressor genes.The epidermal growth factor receptor (EGFR) regulates cell proliferation, apoptosis, angiogenesis, and tumor invasion. Mutations and amplification of EGFR are common in non-small-cell lung carcinoma and provide the basis for treatment with EGFR-inhibitors. Her2/neu is affected less frequently. Other genes that are often mutated or amplified are c-MET, NKX2-1, LKB1, PIK3CA, and BRAF.
The cell lines of origin are not fully understood.The mechanism may involve abnormal activation of stem cells. In the proximal airways, stem cells that express keratin 5 are more likely to be affected, typically leading to squamous-cell lung carcinoma. In the middle airways, implicated stem cells include club cells and neuroepithelial cells that express club cell secretory protein. Small-cell lung carcinoma may be derived from these cell lines or neuroendocrine cells,and may express CD44.
Metastasis of lung cancer requires transition from epithelial to mesenchymal cell type. This may occur through activation of signaling pathways such as Akt/GSK3Beta, MEK-ERK, Fas, and Par6.
 Female Cancer Specialist Doctor in Kanpur female, doctor, cancer, specialist, female, oncologist, oncology, medical, oncologist, chemotherapy, breast, blood, mammography, prostate, center, hospital, radiotherapy, surgery, mouth, kanpur, sn, memorial, female, doctor, cancer, specialist,
Female Cancer Specialist Doctor in Kanpur female, doctor, cancer, specialist, female, oncologist, oncology, medical, oncologist, chemotherapy, breast, blood, mammography, prostate, center, hospital, radiotherapy, surgery, mouth, kanpur, sn, memorial, female, doctor, cancer, specialist,